In Brief
Healthcare consumers are becoming more empowered to have healthcare on their terms. With telemedicine, mobile apps and outpatient centers, patients can receive high-quality care that is convenient and low cost. While emergency departments (ED) provide high-quality care, the long wait times and high cost of care often leave patients frustrated. At the same time, as value-based payment models replace fee-for-service models, hospitals must do more to manage care in the appropriate setting in order to drive down costs.
Considering that approximately 70 percent of hospital admissions enter through the ED, addressing the needs of these patients and lowering the cost of care in this area can have a significant impact across an organization. ED case management programs can do just that.
Benefits of an ED case management program:
- Improved patient experience
- Improved patient throughput
- Increased adherence to new regulatory requirements
- Increased capacity (backfill)
- Reduced denials, inpatient (IP) length of stay (LOS) and 30-day readmissions
- Prevented inappropriate admissions
- Reduced ED length of stay (LOS)
- Managed observation patients (OBS) and high-use patients more efficiently
- Increased correct status (inpatient, outpatient and observation) determination upon admission
The Role of the ED Case Manager
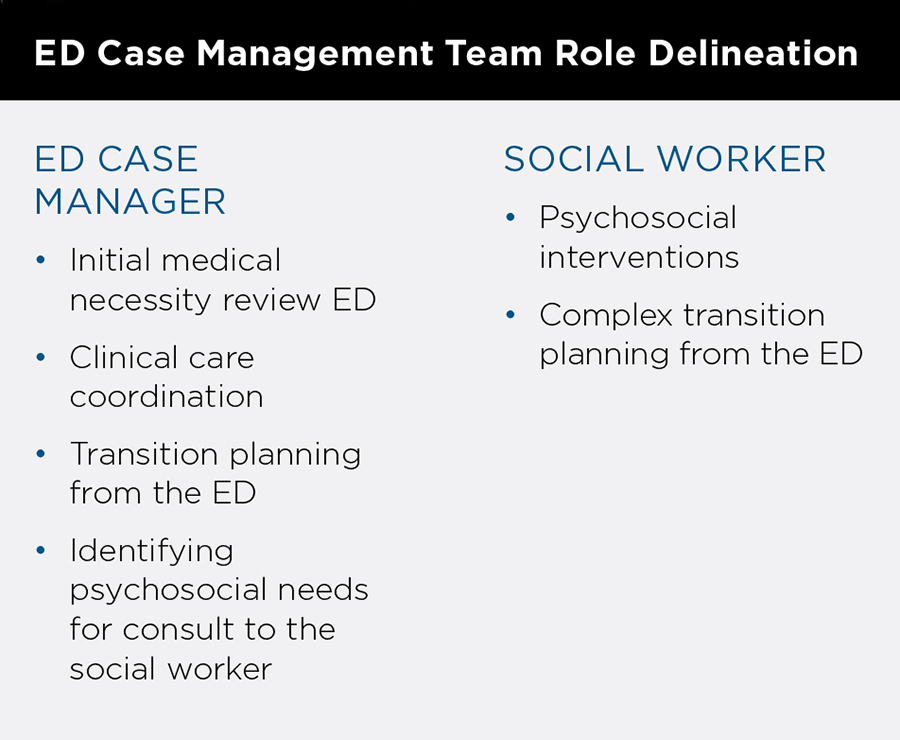
The ED case manager is responsible for an initial medical necessity review for admitted patients and transition planning. Since ED volumes fluctuate significantly, staffing of case managers must account for the time it takes to complete various tasks at a given point in time rather than staffing on a patient-beds ratio. It is also important to assess if a case manager is needed around the clock or if 12 or 18 hours of coverage is adequate.
Initial Medical Necessity Review
As hospitals increase their focus on revenue and patient flow in an effort to improve utilization, initial medical necessity reviews are critical as they help determine the appropriate initial placement for patients. During these reviews, the ED case manager should use an approved tool (e.g., InterQual, MCG) to help assess the appropriate admission status (inpatient or observation). This reduces future changes to status level of care needed post-ED discharge (e.g., acute, intermediate, critical).
Delays in status determination often occur when critical documentation, including diagnostic test results, are unavailable at ED admittance. To avoid these delays the ED case manager should speak to an ED provider to understand their clinical impression of the case. This will provide them with the information needed to discuss the expected treatment period, and appropriate admission status and level of care with the admitting provider in order to complete the initial medical necessity review. When a lack of consensus regarding the appropriate admission status and/or level of care occurs the case manager should contact the designated physician advisor who provides insight on the case.
Transition Planning
ED case managers should collaborate with ED social workers to create patients’ discharge plans. There are many effective models for discharge planning. Best practices include:
- A social worker performs transition planning for patients with complex psychosocial needs.
- A house case manager and/or social worker performs discharge planning after admission for patients who are admitted from the ED.
- An ED case manager performs simple transition planning, when necessary.
Following these best practices ensures that all employees are practicing at the top of their license.
Transition planning from a team of ED case managers and ED social workers can involve assistance with setting up equipment and medication, home health referral and post-acute facility transfers. The team should collaborate with the ED provider to understand the expected needs of the patient and provide recommendations for safe transition plans to prevent inappropriate inpatient admissions. While many physicians do not feel confident in addressing the social needs of patients and may not have the capacity to do so in the fast-paced ED environment, collaboration with this team can fill that gap and provide patients with a strong network of resources to reduce risks of repeat ED visits. Approximately 40-50 percent of readmissions are caused by lack of resources and social problems. As a result, it is critical to discharge patients from the ED with appropriate resources and services that mitigate the risk of readmission.
Manage High-Use Patients
Under value-based payment models, providing the appropriate type of care in the appropriate setting becomes increasingly important. Many patients who are high users of ED services do not need this high level of care and as a result hospitals must try to redirect these patients to other care settings. ED case management programs can put a plan in place that will do just that.
The first step that must be taken is to establish criteria that defines a high user. Then, when a patient who meets high user criteria is admitted, they would automatically be flagged in the EHR.
The ED case manager and social worker should manage high-user patients together, as psychosocial causes often contribute to frequent ED visits. By working together to create a comprehensive post-discharge care plan that includes primary care coordination, insurance enrollment, transportation and housing arrangements, they can address the patient’s medical and psychosocial needs. If the patient returns, this care plan should be reassessed to ensure the patient is receiving the appropriate coordinated services, beyond medical care, to reduce their ED use.
Address Regulatory Changes
Hospitals are facing increased pressure from the Centers for Medicare and Medicaid Services (CMS), state and commercial payers to provide the highest quality and most cost-effective care to patients. The Medicare Conditions of Participation (CoP) outlines the responsibility of the hospital in assuring medical necessity for admission and appropriate level of care and LOS. The CMS CoP applies only to Medicare and Medicaid beneficiaries, but Medicare Advantage and commercial providers often attempt to invoke these regulations.
Regulatory issues that impact ED processes:
- CMS Two Midnight Rule
- Admission begins when physician order is written
- Documentation should include expectation of two midnights and justification (medical necessity)
- Status (IP, OP, OBS) must be ordered
- CMS Condition Code 44
- Issued when a patient is placed in IP status and subsequently changed to OBS based upon medical necessity
- Medicare Outpatient Observation Notice (MOON)
- Notification to patient that they are in an outpatient observation status
- Emergency Medical Treatment and Active Labor Act (EMTALA)
- Medical screening required regardless of their ability to pay or insurance status that is required before disposition from the ED
ED Case Management Metrics
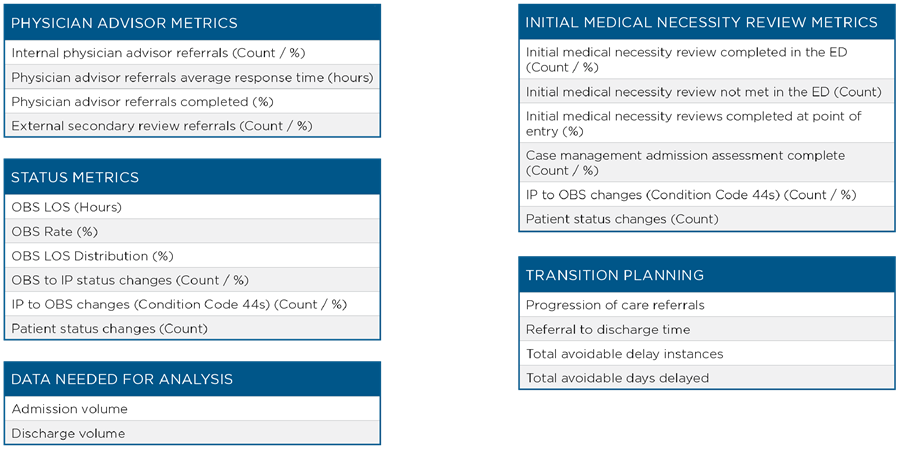
Metrics are essential to monitor the impact of the ED case manager role. It is a best practice role to implement a robust set of metrics. A sample list of metrics include:
Technology Enhancements to Support ED Case Management
Information Technology (IT) plays a critical role in streamlining the ED case management processes by improving communication across the care team. Examples of IT enhancements include:
- Use icons on the ED tracking board to:
- Notify case managers of potential to admit
- Inform ED provider of the case manager’s recommended status for a patient
- Identify out of network patients
- Notify admitting physician of recommended status in the electronic health record (EHR)
ED Case Management Success
By improving the patient experience and providing the appropriate level of care to each patient, patients and hospitals will benefit. Successful case management programs will:
- Better manage frequent ED users.
- Expand patient/family knowledge and understanding of insurance coverage.
- Improve correct status determination upon admission leading to reduced re-work for inpatient case managers and a decline in missed revenue from cases where the correct status is not determined in time.
- Improve patient placement to the correct unit, reducing unnecessary transfers and interruptions to patient care.
- Reduce denials related to medical necessity and level of care.
- Reduce 30-day readmissions.
- Reduce unnecessary admissions from the ED.
Expanding Case Management
While the majority of inpatients, enter through the ED, other entrypoints also benefit from case managers. Patients enter as direct or surgical admissions or through the transfer center, interventional radiology service area, and cardio catheterization and gastroenterology labs. After assessing admission volumes from each entrypoint, hospitals can determine where case management coverage will provide the greatest potential impact.
Hospitals must determine if ED case managers should also cover these additional entrypoints or if separate case managers should be hired.
This assessment must be made by looking at the admissions volumes from the entrypoint, the total scope entrypoint coverage and assessing if the ED case management program’s staffing model/coverage is appropriate for that area.
ED case management programs are a win-win for patients and healthcare organizations. By better assessing patient’s initial care needs and also preparing patients for discharge, patients will be provided with the right care at the right time. This will increase patient satisfaction and lower the cost of care which will be critical as payment models shift. As organizations look to optimize their business today, ED case management programs provide the framework for doing just that.