In Brief
- The sustained financial pressures faced by AMCs require them to reexamine how success is measured and supported across the tripartite mission of clinical care, research, and education.
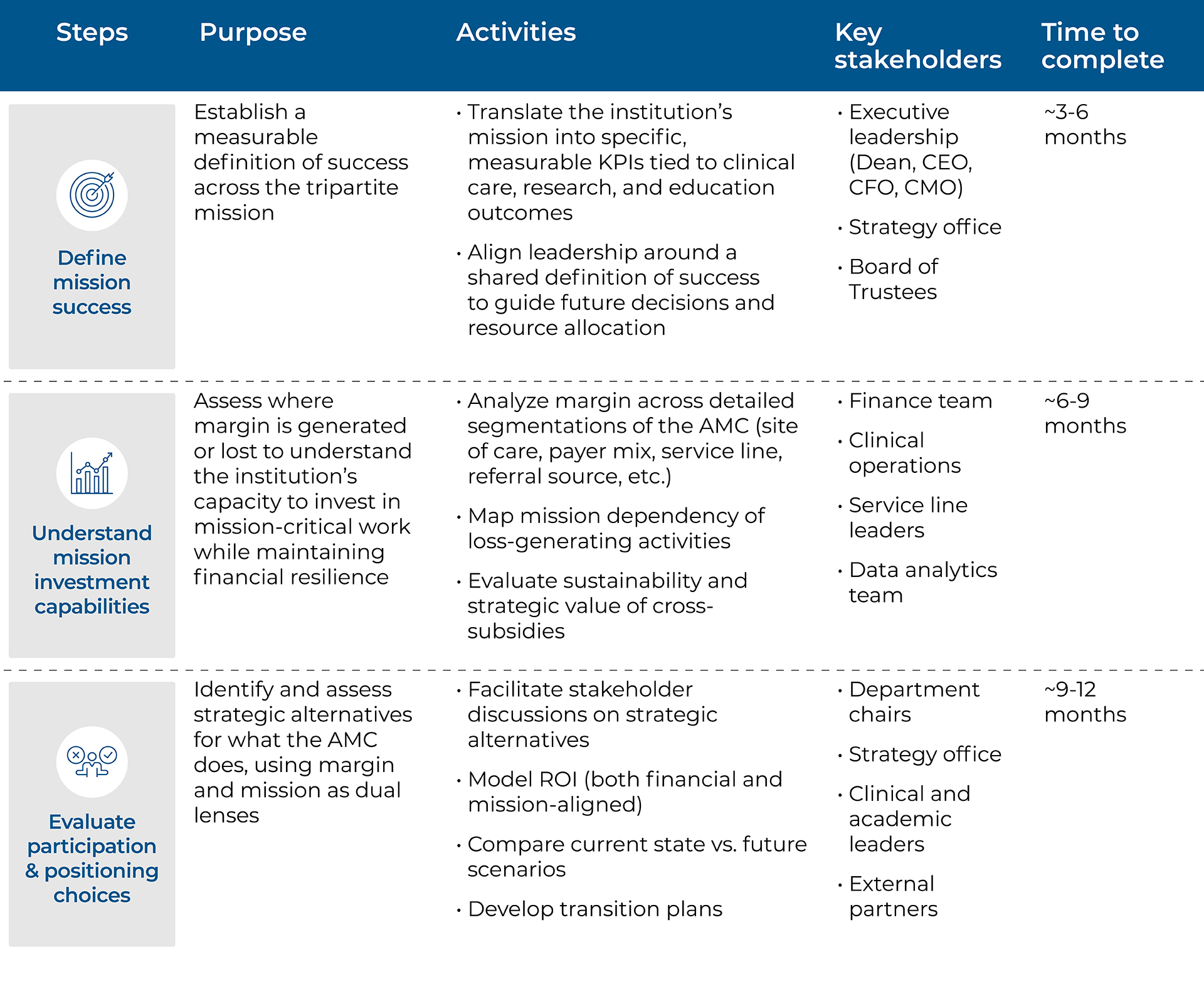
- A structured approach begins with defining mission success, understanding the margin-generating capacity of institutional activities, and optimizing participation and positioning strategies.
- This disciplined process empowers AMCs to adapt, lead, and ensure long-term sustainability in a rapidly changing landscape.
This article is an executive summary of our white paper on supporting AMCs’ tripartite mission in a rapidly changing landscape. You can download the white paper at the link here.
Sustaining the tripartite mission
Academic medical centers operate at the intersection of clinical care, research, and education. The clinical mission provides the financial backbone, enabling cross-subsidization of the other two missions. However, clinical margins have been under increasing pressure due to structural and operational challenges. The research mission, while essential for innovation, often requires institutional subsidies beyond external funding. The decrease in federal funding for research will require further subsidization of the mission. Similarly, the education mission is critical for training future healthcare professionals, but funding constraints have made it increasingly difficult to sustain. These pressures necessitate a strategic reevaluation of how AMCs define success and allocate resources across their tripartite mission.
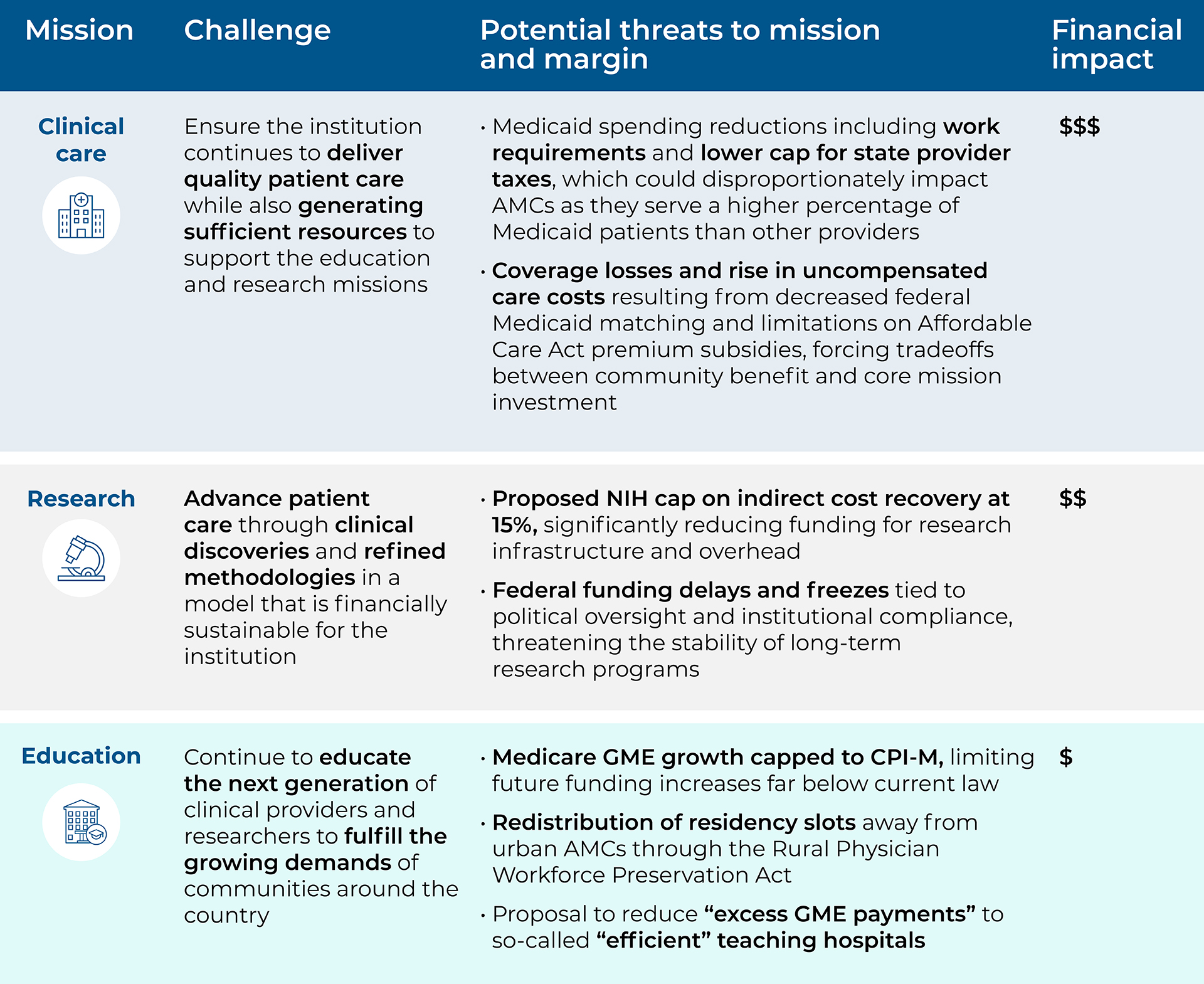
To illustrate the scale and complexity of what lies ahead, the table below outlines the key threats facing each component of the tripartite mission and serves as a snapshot of emerging policy risks. This paper explores how AMCs should consider navigating the industry disruption and sustaining the tripartite mission.
A path forward for AMCs
To thrive amidst the disruption across the industry, AMCs should first develop a clear understanding of what mission success looks like, defining what it means to advance all three mission areas.
Aligning on mission success is a necessary step toward prioritizing mission-critical activities. Next, institutions should understand their investment capacity by identifying which activities generate a sustainable margin that can be reinvested in mission-driven priorities. Finally, AMCs should regularly revisit key participation and positioning choices, encouraging AMCs to reevaluate the activities they engage in (participation choices) and how they differentiate themselves within the academic medicine landscape (positioning choices) — to maximize financial performance and ensure long-term success.
Defining mission success
Even in times of financial constraint, AMCs need to remain deeply focused on activities that directly support their strategic priorities and mission. This is understandably challenging: AMCs’ missions are broad and ambitious, and financial, human, and operational resources are never unlimited. AMCs need to make deliberate choices about where to direct energy, talent, and investment to achieve meaningful impact. Without a distinct and explicit definition of mission success, established at the institutional level, AMCs risk mission creep, gradually expanding into activities that, while well-intentioned, dilute impact and divert resources. Clear, organizationwide definitions of success provide a necessary framework for prioritization, helping institutions stay anchored in their most essential contributions and measure progress in a meaningful way.
Defining mission success requires confronting real and difficult tradeoffs, such as:
- In clinical care: Prioritizing behavioral health services versus expanding advanced cancer therapeutics.
- In research: Focusing on foundational neuroscience discoveries versus scaling applied health services research to address care disparities.
- In education: Investing in interprofessional simulation training versus growing rural physician pipeline programs.
These are not binary or short-term decisions; they are strategic choices that shape the institution’s direction and define its mission responsibilities. What an institution chooses to deprioritize is equally important as what it chooses to prioritize. In a resource-constrained environment, the courage to deprioritize is essential for long-term mission integrity and financial resilience.
Understanding mission investment capabilities
Too often, mission and strategy remain high-level and aspirational, without clearly identifying the measurable outcomes an institution is striving to achieve. Mission success needs to be specific enough to guide action. Mission success clarity is essential not only for aligning organizational efforts but also for understanding the level of financial resilience required to sustain mission investment over time.
To understand the level of financial resilience needed to fund mission success, AMC leaders should have a clear understanding of which activities generate a positive margin and which activities rely on that margin.
Often, positive margins are concentrated within specific subsegments of an institution’s operations. These positive margins emerge when analyzing financials at a detailed level across dimensions such as:
- Payer type
- Case mix index
- Site of care
- Clinical service
- Patient demographics
- Referral source or channel
With this insight, AMC leaders can begin to assess the institution’s business model: Which activities are paying for others? Is that balance intentional, sustainable, and aligned with our mission? The institution’s capacity to ensure margin-generating activities reliably support mission-critical but not self-sustaining activities is a key indicator of performance and financial resilience. Achieving this balancing act requires deliberate, strategic choices.
Evaluating participation and positioning choices
Once AMC leaders have achieved clarity on where positive margin is generated and which activities rely on that value to sustain mission-driven work, they should turn their attention to participation and positioning. Participation choices are the decisions an institution makes about which services, programs, and partnerships it chooses to support. Positioning choices are the decisions an institution makes about how to deliver its services, programs, and partnerships. These choices are the primary levers for optimizing mission investment capability.
Participation and positioning are not static; they should continually evolve in response to internal priorities and external market dynamics. AMCs across the industry are adapting their participation models, expanding into new offerings, and repositioning how they engage patients, learners, and partners to remain relevant and financially viable in a rapidly shifting landscape. Below are examples of how institutions are making these strategic adjustments in practice.
- Geography: Wake Forest Medicine has established a new academic campus in Charlotte’s innovation district, bringing a four-year medical school to what had been the largest U.S. city without one.1
- Services: Indiana University Health sold its health plan to Elevance Health, shifting additional focus to a new operating model that improves patient care models and better supports future growth in expanded footprints.2
- Offering: Cleveland Clinic partnered with Amazon’s One Medical for primary and specialty care in Northeast Ohio, offering same- and next-day appointments, onsite lab services, and wrap-around virtual care support for members.3
- Pricing: The Ohio State Wexner Medical Center announced a new partnership with Sidecar Health to implement a new fixed price model that will increase price transparency for consumers.4
These examples illustrate how intentional participation and positioning choices can unlock new value. To guide similar decisions, AMC leaders should consider participation questions such as:
- Do our initiatives reflect the priorities and needs of our surrounding community? Are we effectively addressing these priorities?
- Which partnerships can help us extend our mission without duplicating investment or infrastructure?
- Are we participating in the right geographic markets to grow sustainably and meet needs?
- How should we engage patients (e.g., hospital-based, ambulatory, digital, or community-based)?
- Are we prioritizing research initiatives aligned with our long-term goals and available funding?
AMC leaders should equally consider positioning questions such as:
- What distinguishes our institution’s contributions, and are we investing accordingly?
- Are we using digital tools to improve clinical reach, research collaboration, and learner access?
- How does our experience with patients, learners, and research collaborators shape our brand in the market?
- Are care delivery, research, and teaching functions siloed? How could our operating model foster integration?
Change process
Reimagining your AMC for long-term sustainability isn’t easy. It takes time, focus, and collaboration across the enterprise. But it’s a necessary investment — one that will unlock greater capacity and future success. The following framework is designed to guide you through the process, illustrating the structured three-step process outlining the purpose, key activities, stakeholders, and expected timelines for each step.
A strategic plan with specific, measurable goals is foundational for an AMC to understand the financial resilience required to sustain its mission investments over time. Sustaining those mission investments depends on a thorough understanding of which local activities generate positive margin and how those resources support mission-critical priorities. This financial insight empowers institutions to optimize their mission investment capacity and mission impact by making deliberate participation and positioning choices, deciding where to engage and how to deliver value. Through this disciplined approach, AMCs can ensure long-term sustainability while advancing their core academic, clinical, and research missions in an evolving healthcare landscape.
Read our white paper on supporting AMCs’ tripartite mission in a rapidly changing landscape.
Huron knows AMCs
Huron has collaborated with over 800 health systems, including 93 of the 100 largest hospitals and health systems in the U.S., to help institutions navigate complex questions related to participation, strategic positioning, and financial sustainability. We support mission critical decisions and enterprise-wide transformations that enable institutions to adapt to the rapidly evolving healthcare landscape.
If you are ready to explore how to sustain your AMC’s tripartite mission while tackling today’s challenges head-on, we invite you to contact us.
- Lee Smith, managing director
- Rick Rohrbach, managing director
- Buffy Kelly, managing director
Neal Houston, Jackson Nell, Nick Grimmer, Jane Doherty, and Allison Murphy contributed to this article.
Endnotes
- Wake Forest News, Wake Forest expands to Charlotte’s Innovation District, marking historic milestone in education, https://news.wfu.edu/2025/06/06/wake-forest-expands-to-charlottes-innovation-district-marking-historic-milestone-in-education/, accessed July 16, 2025.
- Becker’s Hospital Review, “IU Health sells health plan to Elevance,” January 2, 2025, https://www.beckershospitalreview.com/finance/iu-sells-health-plan-to-elevance/, accessed June 6, 2025.
- Cleveland Clinic Newsroom, “Cleveland Clinic and Amazon One Medical Announce Collaboration to Expand Access to High-Quality Coordinated Care in the Cleveland Area,” October 21, 2024, https://newsroom.clevelandclinic.org/2024/10/21/cleveland-clinic-and-amazon-one-medical-announce-collaboration-to-expand-access-to-high-quality-coordinated-care-in-the-cleveland-area/, accessed June 6, 2025.
- Becker’s Payer Issues, “OSU Wexner, startup payer partner on transparent pricing model,” December 19, 2024, https://www.beckerspayer.com/payer/osu-wexner-startup-payer-partner-on-transparent-pricing-model/, accessed June 6, 2025.
Supporting sources
Huron, independent analysis of operating margins of health systems within 20 leading AMCs, (2018-2023).
Centers for Medicare & Medicaid Services, Fiscal Year 2024 Financial Report, 2024, https://www.cms.gov/files/document/cms-financial-report-fiscal-year-2024.pdf, accessed May 31, 2025.
U.S. Senate Committee on Finance, Ways and Means Committee, 2025, https://www.finance.senate.gov/imo/media/doc/budget_optionspdf.pdf, accessed May 31, 2025.
U.S. House of Representatives, Committee on Energy and Commerce, Majority Memorandum for May 13, 2025, Committee on Energy and Commerce Markup, May 11, 2025, https://docs.house.gov/meetings/IF/IF00/20250513/118261/HMKP-119-IF00-20250513-SD003.pdf, accessed May 31, 2025.
Kaiser Family Foundation, “Putting $880 Billion in Potential Federal Medicaid Cuts in Context of State Budgets and Coverage,” May 2025, https://www.kff.org/medicaid/issue-brief/putting-880-billion-in-potential-federal-medicaid-cuts-in-context-of-state-budgets-and-coverage/, accessed May 31, 2025.
Definitive Healthcare, “Medicaid Patient Revenue at AMCs vs. Non-AMCs,” 2025, https://www.defhc.com/, accessed May 31, 2025. Note: Huron analysis included comparing across all AMCs in the 2025 database and non-AMCs.
American Hospital Association, “Fact Sheet: Hospital Impacts of Capita Cap on Medicaid Expansion Population,” May 1, 2025, https://www.aha.org/fact-sheets/2025-05-01-fact-sheet-hospital-impacts-capita-cap-medicaid-expansion-population/, accessed May 31, 2025.
Peter G. Peterson Foundation, “What Is Site Neutrality and Could It Help Reduce Healthcare Costs?” 2024, https://www.pgpf.org/article/what-is-site-neutrality-and-could-it-help-reduce-healthcare-costs/, accessed May 31, 2025.
Weiland, N., and S.G. Stolberg, “N.I.H. to Cap Indirect Cost Payments on Grants, Sparking Uproar from Universities,” The New York Times, April 4, 2025, https://www.nytimes.com/2025/04/04/us/politics/nih-medical-research-funding.html, accessed May 31, 2025.
National Institutes of Health, RePORTER Database, https://reporter.nih.gov/, accessed May 31, 2025. Note: Huron conducted analysis of FY24 NIH Funding by School Type.
Salcedo, A., “Columbia to Lay Off Nearly 180 Researchers Funded by Federal Grants,” Columbia Daily Spectator, May 6, 2025, https://www.columbiaspectator.com/news/2025/05/06/columbia-to-lay-off-nearly-180-researchers-funded-by-federal-grants/, accessed May 31, 2025.
Harvard T.H. Chan School of Public Health, “Trump Administration Freezes $2.2 Billion in Grants to Harvard,” 2025, https://hsph.harvard.edu/news/trump-administration-freezes-2-2-billion-in-grants-to-harvard/, accessed May 31, 2025.
Health Resources and Services Administration, Projecting Health Workforce Supply and Demand, 2024, https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-demand/, accessed May 31, 2025.
Mullan, F., Chen, C., and Steinmetz, E., “The Geography of Graduate Medical Education: Imbalances Signal Need for New Distribution Policies,” Health Affairs, 2006, https://pmc.ncbi.nlm.nih.gov/articles/PMC1466620/, accessed May 31, 2025.
Association of American Medical Colleges, “Addressing the Physician Workforce Shortage, 2024,” https://www.aamc.org/advocacy-policy/addressing-physician-workforce-shortage/, accessed May 31, 2025.
U.S. Government Accountability Office, “Graduate Medical Education: Opportunities to Better Ensure Transparency, Effectiveness, and Accountability, GAO-21-391,” July 2021, https://www.gao.gov/assets/gao-21-391.pdf (see Appendix I), accessed May 31, 2025.
Congressional Budget Office, “Options for Reducing the Deficit: 2025 to 2034,” December 2024, https://www.cbo.gov/system/files/2024-12/60557-budget-options.pdf, accessed May 31, 2025.
Bureau of Labor Statistics, Consumer Price Index (CPI) Databases, 2025, https://www.bls.gov/cpi/, accessed May 31, 2025.
NSF HERD Survey, “Higher education R&D expenditures reported by all institutions (standard form and short form populations),” https://ncses.nsf.gov/surveys/higher-education-research-development/2023#data, accessed June 25, 2025.
U.S. Department of Health and Human Services, ED, HHS, and GSA Initiate Review of Anti-Semitic Activity at the University of Washington, https://www.hhs.gov/press-room/anti-semitism-task-force-statement-on-university-of-washington.html, accessed June 27, 2025.