In Brief
Increase physician engagement, optimize performance while transforming to value-driven growth.
As value-driven growth models replace fee-for-service payment plans, healthcare organizations are taking on increasingly complex payment and reimbursement plans. Leaders are struggling to align their system’s financial and quality goals with those of physicians, while balancing the increasing demands and stresses on physicians and their patient care teams. Physicians and advanced practice providers are crucial to performance, quality, safety, care utilization and patient satisfaction goals, all of which impact an organization’s financial viability. This is why providers’ compensation must be aligned with them. In addition, our research shows that providers are less likely to burn out when mutual goals have been established between them and their health systems.
Compensation Structure Versus Organizational Culture
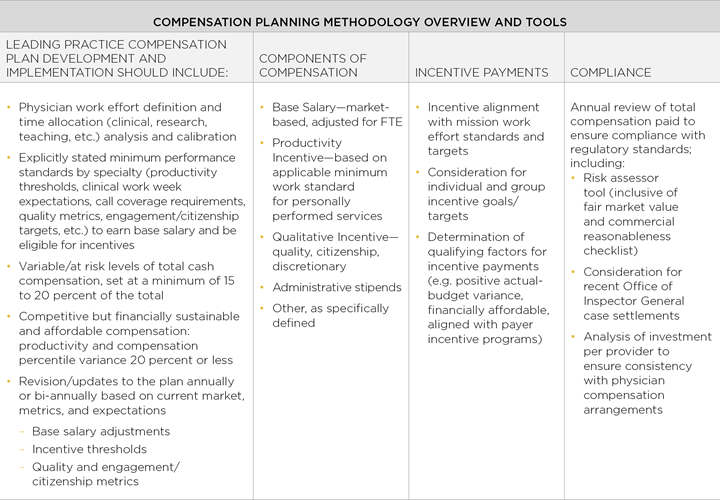
The right compensation plan framework is an important component to becoming a high-performing physician organization. It provides a tangible and aligned structure for a winning strategy that benefits patients, providers and payers. Creating a unified plan also helps integrate providers with each other and with the system via a common core that functions across multiple departments, but is flexible enough to contain specific departmental metrics, variables and incentives. Ultimately, this framework should facilitate a bridge to a more risk based, population health focused care delivery system as you gradually realign measures, metrics and compensation to value-driven growth models.
A compensation structure is also dependent on a physician organization’s culture and dynamics. Leaders should ask these questions:
- Where does your organization fall on the organizational maturity spectrum?
- Are the physicians ready and motivated to move to a unified and aligned compensation plan?
- Can this plan evolve and be repeated with other physician groups or will you need to tailor the structure for each group you employ, thus defeating the implementation of a unified plan?
A unified compensation structure with common principles and guardrails is important and should be pursued, but does not insinuate that a one-size-fits-all approach is effective or even feasible. Rather, successful physician organizations should develop common principles that will apply broadly to all providers, but with specialty or group specific components that give leaders flexibility to meet the needs of individual physicians and the physician organization. For example, common principles may be rewarding for patient satisfaction or a range of fixed and variable compensation.
Alignment Among Many Sectors
Compensation plans must be financially sustainable, reward physicians for meeting and exceeding clinical and nonclinical goals, and balance physician efforts with a variety of leadership responsibilities. Above all, approach compensation planning with transparency and accountability, and keep things simple and efficient.
Successful compensation plans are works in progress and should account for:
- Patients, consumers, community: Encompassing population health, which determines what the prevalent chronic and acute illnesses in your market are, the rise of consumerism, multiple patient access channels including telehealth and retail clinics, and the impact of self-payers.
- Health systems: Representing the continuum of care across the delivery system including hospitals, academic medical centers, ambulatory practices and post-acute environments.
- Government: Including federal, state and local laws and policies that regulate your organization’s operation.
- Payers: Reimbursement is continuing to progress on the path to value especially with the Department of Health and Human Services’ goal of tying 50 percent of Medicare fee-for-service payments to quality or value through alternative payment models by 2018.1
Overall Market Dynamics
There has been a marked shift from independent medical groups to hospital-employed/owned physician organizations in the last fifteen years and the trend continues.2 Mergers and acquisitions create their own compensation dynamics. Often these deals are done one at a time, without a complete evaluation of the strategic goals and return on investment of all parties.
Physician organizations acquired in this way are promised autonomy, but since their legacy compensation plans often come with them, they are less inclined to embrace the parent health system’s compensation structure. The misalignment perpetuates itself as systems grow and acquire more medical groups. Though hospitals no longer employ physicians to increase admissions and gain favorable reimbursement rates for hospital-based services, the shift from fee-for-service to value-driven growth creates a new dynamic. For compensation planning, there is a need to recognize the impact that an evolving organizational structure has on staff and continue to develop models that reward quality and cost reductions.
Impact of Physician Burnout
Relentless changes and the uncertainties of industry reform are driving physicians to join hospital groups because they no longer want the administrative details of owning a practice and they prefer medicine to business. However, when physicians make the move, they discover that they are needed as leaders on the business side of healthcare.
When physicians experience the disconnect between why they joined a hospital medical group and what the hospital needs from them, their disillusionment can lead to burnout. Burnout factors can be grouped by healthcare environment, practical hurdles, psychological and training challenges, and organizational structure changes. One of these factors can perpetuate others as practical hurdles lead to psychological concerns and training challenges related to organizational change. Burnout is not happening only because physicians feel personally overwhelmed or stressed which would imply a lot of self-interest.
Rather, this dedicated group experiences burnout because their ability to provide the best possible patient care is being challenged. When physicians team up with their health system leaders to pursue mutual goals, they are far less likely to burn out.3
Healthcare system leaders are realizing the importance of getting physicians to align strategically with goals to improve key performance areas such as revenue, care redesign and efficiency, but ignoring burnout limits any physician engagement.4 A variety of strategies can combat the problem including education and onboarding activities, working on patient care teams with non-physician providers to help spread out work and documentation, training physicians to become team leaders, and helping physician organizations become more successful in lowering costs and improving quality of care.
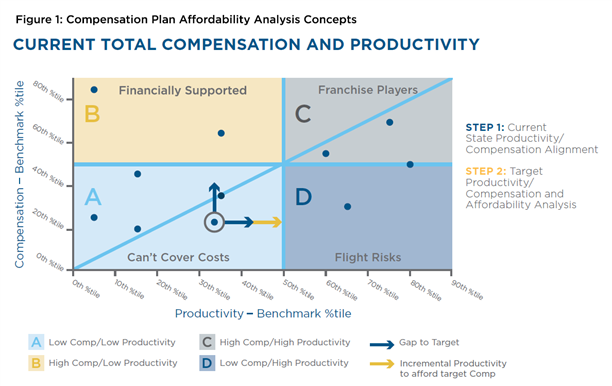
Critical to understanding the relationship between performance expectations/compensation and how physician organizations can become disconnected from the health system is the financial affordability of physicians that can be assessed by looking at total compensation in comparison to productivity (Figure 1). Although health systems recruit, retain and incentivize physicians for any number of clinical or strategic reasons, it is important to continuously evaluate the relationship between productivity and compensation.
Huron’s best practice for financial sustainability and affordability is no more than a 20 percent variance (positive or negative) in the respective percentiles for productivity and compensation. Misalignment greater than 20 percent puts physician organizations at risk for either losing providers or overpaying for them. Strategic or coverage needs may occasionally call for variances outside of this leading practice but should be the exception rather than the rule.
Alignment With High-Performing Groups
Physicians who belong to high-performing organizations significantly impact their health systems both operationally and clinically. This makes for strong partnerships and improved financial performance. In our definition, high performing physician organizations must have sustainable performance as it relates to compensation across these key dimensions:
Organizational Effectiveness
- Effective governance and management structure to successfully develop and implement a leading practice compensation model
- Strong group culture and ethos to buy into market-driven models and incentives
Practice Efficiency
- Highly efficient and appropriately staffed operations
- Able to respond to and track changes driven by new provider incentives
Financial Sustainability of Plan
- Financially viable to health system
- Funded consistently and fairly
- Reporting and transparency for compensation model changes
Provider Alignment
- Compensation is aligned between provider performance and organizational goals including volume, outcomes and cost
Clinical Alignment
- Effective compensation model addressing primary care, specialty care and hospital services
- Incentives aligned with desired system and payer outcomes including performance, quality, utilization, safety and patient satisfaction
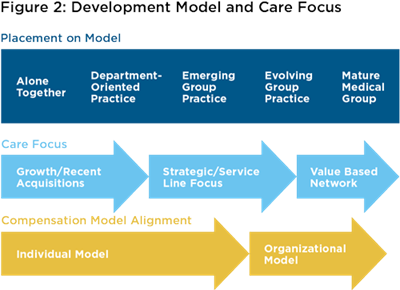
Where a physician organization is at on the journey toward high performance can limit the ability to design and implement a compensation plan for its members. For example, an organization could be an emerging group practice, but its clinical, operational and financial infrastructures are not in line with its culture, values, strategy, leadership and management.
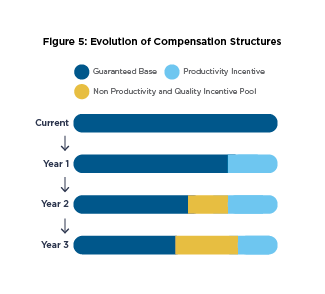
Compensation Approaches
With that in mind, there are several approaches to compensation (Figure 3) ranging from increasingly guaranteed compensation to increasingly variable compensation. Best practice suggests a model where no more than 80-85 percent of a provider’s total cash compensation target (e.g., 50th percentile Medical Group Management Association) is fixed or guaranteed with potential exceptions for new providers during the one-to- two-year ramp-up period. The remaining variable compensation, should be earned based on achieving and/or exceeding minimum work standards/thresholds for productivity, quality and engagement/citizenship. Incentive compensation can then be structured for providers going above and beyond the minimum work standards, giving high achievers the ability to earn more than the total cash compensation target.
Quality and citizenship requirements should always be part of physician leadership onboarding and/or training so physicians know exactly how the organizational culture translates into care delivery performance. There should be minimum expectations for citizenship goals within the physician group and the hospital or healthcare system. Citizen goals can include engaging in leadership opportunities, getting along with peers, having good charting habits and minimizing compliance risks.
Other compensation considerations include physician roles in administrative, management, leadership and other variable pay that should be part of performance metrics. Be sure to make physicians aware of all the quality, citizenship and leadership opportunities your organization offers.
For specialty physician organizations, compensation plan components and incentive metrics should be tailored to the specific group and provider environment, and should ultimately coincide with the goals of each individual practitioner along with those of their department, division and organization.
Key compensation metric guidelines:
- Base compensation on organizational priorities including physician engagement, quality and service line performance, and setting minimum standards for eligibility.
- Calibrate performance expectations per clinical, administrative or other work effort criterion.
- Use external benchmarking data (e.g., Medical Group Management Association).
- Establish a component for not meeting performance expectations.
- Always recognize performance quantitatively and qualitatively.
Compensation Design, Planning and Alignment
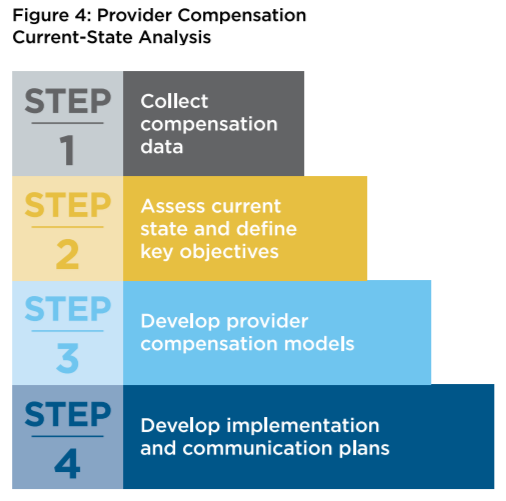
Begin compensation planning by examining current provider models. Complete the four-step process (Figure 4) before starting to develop the goals and key objectives of any new or future compensation plan models.
Kickoff / Data Collection / Business Case
- Gather data and policies around provider compensation and productivity.
- Form a compensation plan work group consisting of key physician and administrative leaders.
- Communicate the need/business case for change with the provider organization, and expectations for input, timing and roll out of potential new plan(s).
Current State Assessment, Development of Guiding Principles and Analysis
- Conduct interviews with physician and administrative leaders to understand what works within the current compensation plan and more importantly, what does not work.
- Perform a benchmarking analysis, comparing current compensation models and affordability.
- Define and develop guiding principles for eligibility, minimum work standards, base salary, incentive compensation and funding.
Compensation Model Design, Testing and Implementation
- Use agreed upon guiding principles to develop department/specialty specific compensation plans.
- Thoroughly “shadow test” by running concurrent calculations of compensation under old and new plans using actual performance data for several months to determine the financial impact, to providers and to the physician organization/ health system, of each option.
- Finalize compensation model components.
- Develop policies and documents.
- The best laid physician compensation plans are meaningless without proper execution of the implementation.
- Establish a communications plan and frequency of communication with providers through monthly newsletters, email updates or surveys.
- Create an implementation work team, work plan and key milestones. Work teams typically include key operations directors and financial analysts.
- Develop and schedule provider.
- Create an implementation work team, work plan and key milestones. Work teams typically include key operations directors and financial analysts.
- Develop and schedule provider education sessions/town hall meetings and model working sessions with the work team.
Key Takeaways
- Evolving provider compensation plans must strike a strong balance in aligning performance including production, quality, citizenship/engagement, variable and at-risk components, incentives, affordability, operational efficiency and provider satisfaction.
- A plan that simply incentivizes providers to work harder without simultaneously engaging and enabling them to be more efficient and effective is destined to fail.
- A plan that focuses on organizational effectiveness, practice efficiency, financial sustainability,and provider and clinical system alignment will create the desired culture of accountability, performance and long term organizational success.
- Develop new patient access channels, optimizing performance, reducing physician burnout, and aligning interests at the provider and system level is paramount to creating a winning environment for patients, physician organizations and health care systems.
- Best practices for designing aligned compensation plans and enabling a high-performing physician organization.
- Develop a common framework compensation plan, allowing for flexibility to meet the needs of various specialties and stages of alignment.
- Design elements in the plan that address shifting reimbursement models.
- Align the framework with health system strategies and goals.
- Ensure the plan is both financially affordable and sustainable.
- Implement the plan in conjunction with operational improvements (e.g. revenue cycle enhancements, productivity/access/throughput standards and expense management) to help physicians succeed.
While marketplace and regulatory demands continue to put pressure on the healthcare delivery system, a carefully considered physician compensation plan can be used to leverage most of the relationships in the care continuum. It not only incentivizes a high-performing physician organization but provides an aligned structure for a winning patient-provider-system-payer strategy.
References
1 https://innovation.cms.gov/initiatives/Health-Care-Payment-Learning-and-Action-Network/
2 “Physicians Continue to Leave Private Practice for Employment,”Jackson Healthcare, June 23, 2015. http://www.jacksonhealthcare.com/media-room/articles/physician-trends/physicians-continue-to-leave-private-practice-for-employment/
3 Studer, Quint and Ford, George, MD, Healing Physician Burnout: Diagnosing, Preventing, and Treating, Fire Starter Publishing, 2015.
4 Physician Burnout Extinguishes Physician Engagement,” Becker’s Hospital Review, April 29, 2015. http://www.beckershospitalreview.com/hospital-physicianrelationships/physicianburnout-extinguishes physicianengagement.html